Revolutionizing Healthcare Back-Office Workflows with Cofactor AI
In the dynamic healthcare industry, where financial optimization and operational efficiency are paramount, Cofactor AI emerges as a groundbreaking solution designed to automate and streamline healthcare back-office workflows. This cutting-edge AI-powered platform addresses one of the industry’s most pressing challenges – insurance denial management – by revolutionizing the appeals process.
Cofactor AI’s innovative technology aims to boost the bottom line for healthcare providers by increasing revenue, enhancing efficiency, reducing denials, and accelerating the revenue cycle. By automating the generation of appeal letters, the platform leverages contextual information such as clinical notes, local regulations, insurance plan details, and insights from successful past appeals to craft personalized and compelling submissions. This strategic approach reduces the manual workload involved in claims management by up to 90%, enabling healthcare providers to recapture lost revenue more effectively.
Safeguarding sensitive data and ensuring compliance with industry standards are top priorities for Cofactor AI. The platform employs Vanta, a comprehensive security and compliance monitoring solution, to maintain the integrity of its infrastructure and adhere to best practices across the industry.
How Cofactor AI Simplifies Insurance Denial Management
Cofactor AI’s cutting-edge AI technology streamlines the complex and often cumbersome process of handling insurance denials. Here’s a closer look at the platform’s key features and functionalities:
- Automated Letter Generation: Cofactor AI’s advanced algorithms analyze the details of a denied claim and automatically generate a tailored appeal letter, optimizing the chances of overturning the denial.
- Cofactor Knowledge Augmented GenAI (C-KAG): This innovative feature expedites the process of finding the optimal information needed to appeal a denial, significantly reducing the time required to manage these complex processes.
- Real-Time Appeals: Seamless integration with Electronic Medical Records (EMRs), Clearinghouses, and Payers allows healthcare providers to appeal denials almost instantly, streamlining the denial management workflow.
- Denial Management Solution: Cofactor AI’s comprehensive platform captures, tracks, and organizes every denied claim, ensuring that no claim goes unaddressed and enabling in-depth analysis for improved decision-making.
Transformative Benefits for Healthcare Providers
Cofactor AI’s feature-rich platform delivers a wide range of benefits that can profoundly impact healthcare providers’ operations and financial performance:
- Increased Revenue: By automating the appeals process, healthcare providers can recapture significant revenue from denied claims, directly boosting their bottom line.
- Enhanced Efficiency: Reducing the manual workload by up to 90% leads to a more efficient and streamlined back-office operation, freeing up resources for other critical tasks.
- Streamlined Denial Management: Cofactor AI’s real-time tracking, management, and appeal capabilities enable a more seamless and optimized revenue cycle.
- Security and Compliance: Cofactor AI’s commitment to security and compliance is reinforced by its partnership with Vanta, which provides continuous infrastructure monitoring and adherence to industry best practices.
Unlocking the Potential of Cofactor AI
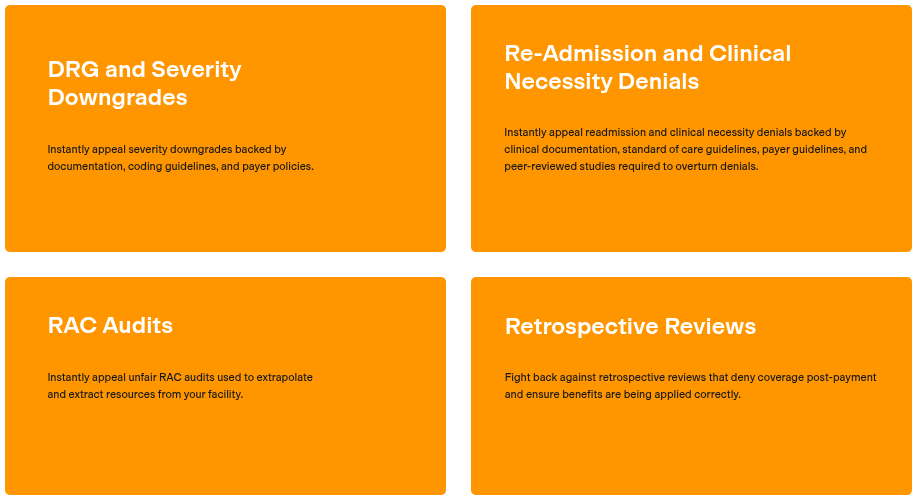
Cofactor AI’s innovative solutions are particularly beneficial in the following use cases:
- Automated Appeals for Denied Claims: Healthcare providers often face a high volume of denied claims, which can be overwhelming to manage manually. Cofactor AI’s automated appeals process makes this task more manageable and less time-consuming.
- Revenue Cycle Management (RCM) Optimization: By streamlining denial management, Cofactor AI enhances the overall efficiency of the revenue cycle, leading to increased revenues and improved financial performance.
- Compliance and Security: In an industry where compliance and security are non-negotiable, Cofactor AI provides an added layer of protection by monitoring its infrastructure according to the most stringent industry standards.
Who Benefits from Cofactor AI?
Cofactor AI’s transformative solutions cater to a wide range of stakeholders within the healthcare industry, including:
- Billing Teams: Billing professionals who manage the complexities of insurance claims and denials can greatly benefit from the automation and efficiency offered by Cofactor AI.
- Healthcare Providers: From small clinics to large hospitals, any healthcare provider that handles insurance claims can leverage Cofactor AI to drive significant improvements in revenue and operational efficiency.
- Claims Managers: Professionals responsible for managing and appealing denied claims will find Cofactor AI’s automated solutions a valuable asset in their day-to-day operations.
To learn more about Cofactor AI and its transformative capabilities, visit their official website at https://cofactorai.com. The website also provides access to additional resources, such as the privacy policy, terms of service, and the trust center, offering insights into the platform’s commitment to security, compliance, and user trust.
Cofactor AI represents a remarkable advancement in healthcare back-office automation, promising to revolutionize the way healthcare providers manage insurance denials and optimize their revenue cycles.